What is sleep apnea?
Sleep apnea is a common but serious sleep disorder where your breathing is briefly interrupted when you’re asleep. If you have sleep apnea, you’re probably not aware of these short breathing pauses that occur hundreds of times a night, jolting you out of your natural sleep rhythm. All you know is that you don’t feel as energetic, mentally sharp, or productive during the day as you should do.
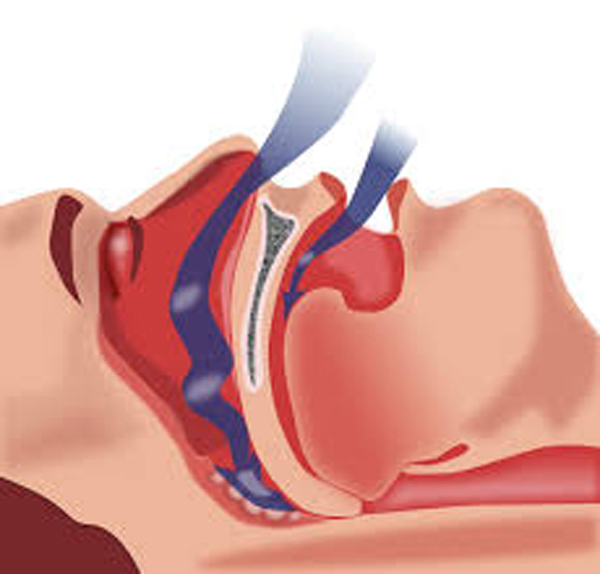
The most common type of sleep apnea—obstructive sleep apnea—occurs when the airway is blocked, causing pauses in breathing and loud snoring. Since sleep apnea only occurs while you’re sleeping, you may only discover you have a problem when a bed partner or roommate complains about your snoring. Though you may feel self-conscious about it or tempted to just make light of your snoring, it’s something you shouldn’t ignore. Sleep apnea can take a serious toll on your physical and emotional health.
The chronic sleep deprivation caused by sleep apnea can result in daytime sleepiness, slow reflexes, poor concentration, and an increased risk of accidents. Sleep apnea can cause moodiness, irritability, and even lead to depression, as well as serious physical health problems such as diabetes, heart disease, liver problems, and weight gain. With the right treatment and self-help strategies, however, you can control your snoring and the symptoms of sleep apnea, get your sleep back on track, and feel refreshed and alert during the day.
Types of sleep apnea
Obstructive sleep apnea is the most common type of sleep apnea. It occurs when the soft tissue in the back of the throat relaxes during sleep and blocks the airway, often causing you to snore loudly.
Central sleep apnea is a much less common type of sleep apnea that involves the central nervous system, occurring when the brain fails to signal the muscles that control breathing. People with central sleep apnea seldom snore.
Complex sleep apnea is a combination of obstructive sleep apnea and central sleep apnea.
Signs and symptoms of sleep apnea
It can be tough to identify sleep apnea on your own, since the most prominent symptoms only occur when you’re asleep. But you can get around this difficulty by asking a bed partner to observe your sleep habits, or by recording yourself during sleep. If pauses occur while you snore, and if choking or gasping follows the pauses, these are major warning signs that you have sleep apnea.
Major warning signs
- Loud and chronic snoring almost every night
- Choking, snorting, or gasping during sleep
- Pauses in breathing
- Waking up at night feeling short of breath
- Daytime sleepiness and fatigue, no matter how much time you spend in bed
Other warning signs
- Waking up with a dry mouth or sore throat
- Insomnia or nighttime awakenings; restless or fitful sleep
- Going to the bathroom frequently during the night
- Forgetfulness and difficulty concentrating
- Uncharacteristic moodiness, irritability, or depression
- Morning headaches
- Impotence
Sleep apnea causes
While anyone can have sleep apnea, you have a higher risk for obstructive sleep apnea if you’re:
- Overweight, male, with a family history of sleep apnea
- Over the age of 50, a smoker, affected by high blood pressure
- Black, Hispanic, or a Pacific Islander
- Someone with a neck circumference greater than 15.75 inches (40 cm)
Other physical attributes that put you at risk for obstructive sleep apnea include a deviated septum, receding chin, or enlarged tonsils or adenoids. Your airway may be blocked or narrowed during sleep simply because your throat muscles tend to relax more than normal. Allergies or other medical conditions that cause nasal congestion and blockage can also contribute to sleep apnea.
Central sleep apnea causes
Like obstructive sleep apnea, central sleep apnea is more common in males and people over the age of 65. However, unlike obstructive sleep apnea, central sleep apnea is often associated with serious illness, such as heart disease, stroke, neurological disease, or spinal or brainstem injury. The first step in treating central sleep apnea is to treat the existing medical conditions that are causing it.
Some people with obstructive sleep apnea can develop central sleep apnea when they’re being treated with positive airway pressure (PAP) devices.
Self-help treatments
While a diagnosis of sleep apnea can be scary, it is a treatable condition. In fact, there are many things you can do on your own to help, particularly for mild to moderate sleep apnea. Home remedies and lifestyle modifications can go a long way in reducing sleep apnea symptoms. However, they should not replace medical evaluation and treatment.
Lifestyle changes to reduce sleep apnea symptoms
Lose weight. People who are overweight have extra tissue in the back of their throat, which can fall down over the airway and block the flow of air into the lungs while they sleep. Even a small amount of weight loss can open up your throat and improve sleep apnea symptoms.
Quit smoking. Smoking contributes to sleep apnea by increasing inflammation and fluid retention in your throat and upper airway.
Avoid alcohol, sleeping pills, and sedatives, especially before bedtime, because they relax the muscles in the throat and interfere with breathing.
Exercise regularly. As well as helping you lose weight, regular exercise can have a major effect on the duration and quality of sleep. Aerobic and resistance training can help reduce sleep apnea symptoms, while yoga is also good for strengthening the muscles in your airways and improving breathing.
Avoid caffeine and heavy meals within two hours of going to bed.
Maintain regular sleep hours. Sticking to a steady sleep schedule will help you relax and sleep better. Sleep apnea episodes decrease when you get plenty of sleep.
Bedtime tips for preventing sleep apnea
Sleep on your side. Avoid sleeping on your back which makes it more likely for your tongue and soft tissues to obstruct your airway. Some people only experience sleep apnea when sleeping on their back.
The tennis ball trick. To keep yourself from rolling onto your back while you sleep, sew a tennis ball into a pocket on the back of your pajama top. Or wedge a pillow stuffed with tennis balls behind your back.
Prop your head up. Elevate the head of your bed by four to six inches, or elevate your body from the waist up by using a foam wedge or special cervical pillow.
Open your nasal passages at night by using a nasal dilator, saline spray, breathing strips, or a nasal irrigation system (neti pot).
Tighten the muscles that keep the mouth closed. Try chewing gum or holding a pen between your teeth for about 10 minutes before bedtime, or until your jaw starts to ache.
Throat exercises
Throat and tongue exercises may reduce the severity of sleep apnea by strengthening the muscles in the airway, making them less likely to collapse. It may take several weeks before you start to notice the benefits.
Try these exercises:
- Press your tongue flat against the floor of your mouth and brush top and sides with a toothbrush. Repeat brushing movement five times, three times a day.
- Press the length of your tongue to the roof of your mouth and hold for three minutes a day.
- Place a finger into one side of your mouth. Hold the finger against your cheek while pulling the cheek muscle in at same time. Repeat 10 times, rest, and then alternate sides. Repeat this sequence three times.
- Purse your lips as if to kiss. Hold your lips tightly together and move them up and to the right, then up and to the left 10 times. Repeat this sequence three times.
- Place your lips on a balloon. Take a deep breath through your nose then blow out through your mouth to inflate the balloon as much as possible. Repeat five times without removing balloon from your mouth.
- Gargle with water for five minutes, twice a day.
- Lightly hold your tongue between your teeth. Swallow five times. Repeat this five times a day.
Sleep apnea treatment options
If your sleep apnea is moderate to severe, or you’ve tried self-help strategies and lifestyle changes without success, a sleep doctor may help you find an effective treatment. Treatment for sleep apnea has come a long way in recent times, so even if you were unhappy with sleep apnea treatment in the past, you may now find something that works for you.
Treatments for central and complex sleep apnea usually include treating any underlying medical condition causing the apnea, such as a heart or neuromuscular disorder, and using supplemental oxygen and breathing devices while you sleep.
Treatment options for obstructive sleep apnea include:
- CPAP
- Other breathing devices
- Dental devices
- Implants
- Surgery
*Medications are only available to treat the sleepiness associated with sleep apnea, not the sleep apnea itself.
Option 1: CPAP

Continuous Positive Airflow Pressure (CPAP) is the most common treatment for moderate to severe obstructive sleep apnea. The CPAP device is a mask-like machine that covers your nose and mouth, providing a constant stream of air that keeps your breathing passages open while you sleep.
If you’ve given up on sleep apnea machines in the past because of discomfort, you owe it to yourself to give them a second look. CPAP technology is constantly being updated and improved, and the new CPAP devices are lighter, quieter, and more comfortable. In many cases, you’ll experience immediate symptom relief and a huge boost in your mental and physical energy.
Option 2: Other breathing devices
In addition to CPAP, there are other devices that a sleep specialist may recommend for sleep apnea treatment:
Expiratory positive airway pressure (EPAP) single-use devices fit over the nostrils to help keep the airway open and are smaller, less intrusive than CPAP machines and may benefit people with mild-to-moderate obstructive sleep apnea.
Bilevel positive airway pressure (BiPAP or BPAP) devices can be used for those who are unable to adapt to using CPAP, or for central sleep apnea sufferers who need assistance for a weak breathing pattern. This device automatically adjusts the pressure while you’re sleeping, providing more pressure when you inhale, less when you exhale. Some BiPAP devices also automatically deliver a breath if it detects you haven’t taken one for a certain number of seconds.
Adaptive servo-ventilation (ASV) devices can be used for treating central sleep apnea as well as obstructive sleep apnea. The ASV device stores information about your normal breathing pattern and automatically uses airflow pressure to prevent pauses in your breathing while you’re asleep.
Option 3: Dental devices
Most dental devices are acrylic and fit inside your mouth, much like an athletic mouth guard. Others fit around your head and chin to adjust the position of your lower jaw. Two common oral devices are the mandibular repositioning device and the tongue retaining device. These devices open your airway by bringing your lower jaw or your tongue forward during sleep.
Dental devices are only effective for mild to moderate sleep apnea. There are also a number of troubling side effects from using this type of treatment, including soreness, saliva build-up, nausea, and damage or permanent change in position of the jaw, teeth, and mouth.
It’s very important to get fitted by a dentist specializing in sleep apnea, and to see the dentist on a regular basis to monitor any problems and periodically adjust the mouthpiece.
Option 4: Sleep apnea implants
One of the newest treatments for sleep apnea involves the insertion of a pacemaker system that stimulates muscles to keep airways open so you can breathe during sleep. The new treatment has been approved by the FDA in the U.S. for people with moderate to severe obstructive sleep apnea.
Although the technology is relatively new (and expensive), studies suggest it may also benefit people with central sleep apnea.
Option 5: Surgery
If you have exhausted other sleep apnea treatment options, surgery can increase the size of your airway, thus reducing episodes of sleep apnea.
The surgeon may remove tonsils, adenoids, or excess tissue at the back of the throat or inside the nose, reconstruct the jaw to enlarge the upper airway, or implant plastic rods into the soft palate. Surgery carries risks of complications and infections, and in some rare cases, symptoms can become worse after surgery.
Sleep apnea in children
While obstructive sleep apnea can be common in children, it’s not always easy to recognize. In addition to continuous loud snoring, children with sleep apnea may:
- Pause breathing while sleeping, snort, or gasp
- Adopt strange sleeping positions
- Suffer from bedwetting, excessive perspiration at night, or night terrors
- Exhibit daytime sleepiness
- Develop behavioral problems or declining grades
If you suspect sleep apnea in your child, it’s important to consult a pediatrician who specializes in sleep disorders. Left untreated, sleep apnea can affect your child’s learning, mood, growth, and overall health.
Causes and treatment for sleep apnea in children
The most common causes of obstructive sleep apnea in kids are enlarged tonsils and adenoids. A simple adenotonsillectomy to remove the tonsils and adenoids usually corrects the problem. Your child’s doctor may also recommend using a CPAP or other breathing device.
If excess weight is causing your child’s obstructive sleep apnea, your support, encouragement, and positive role modeling can help your child reach and maintain a healthy weight—and get your whole family on a healthier track.